|
The Surgical Technologist
|
APRIL 2015
160
ture and other complications such as seroma formation
have decreased considerably in both delayed and immedi-
ate reconstruction patients.
7
Latissimus dorsi flap patients
are immediate or delayed reconstructions following simple
or modified radical mastectomy.
The vast majority of delayed reconstructive patients
have undergone radiation as part of their chosen cancer
treatments in addition to one or two mastectomies. The
processes of irradiating the tissue surrounding the cancer
site leaves significant histological changes to include, but
not limited to, atrophy and atypia of the epithelia, calci-
fication in the fibrous tissue walls and thickening of the
lumen of vessels.
2
R E L E V A N T A N A T O M Y A N D P H Y S I O L O G Y
The latissimus dorsi muscle is a broad flat superficial mus-
cle of the lower part of the back that originates mostly in
a broad aponeurosis attached to the spinous processes of
the vertebrae of the lower back, the supraspinal ligament
and the crest of the ilium, and is inserted into the bicipital
groove of the humerus. It is the largest muscle in the body,
spanning 20 to 40 centimeters, which makes for an ideal
muscle to use in the coverage of extremely large wounds.
In the event of a complex or massive wound the pedicle
can be combined with the serratus, scapular or parascap-
ular flaps to create adequate coverage.
5
Blood supply is
provided by the thoracodorsal artery via the subscapular
artery and nerve innervation is provided by the thoracodor-
sal nerve.
2
The chest muscles lie inferior to breast tissue and the
pectoralis fascia. These muscles are composed of the pecto-
ralis major, the pectoralis minor and intercostal muscles of
the ribs and can cover portions of the anterior serratus mus-
cle. The pectoralis major muscle originates at the anterior
surface of the sternum and inserts into the anterior surface
of the medial half of the clavicle.
3
S U R G I C A L I N T E R V E N T I O N
Positioning and Positioning Aids
This procedure requires equipment for two stages of posi-
tioning. For induction, the patient is placed supine on a
reversed ACMI surgical bed that has been prepared with
the following layers; fitted sheet, bean bag, three-quarter gel
pad, fitted sheet and two chuck pads. The patient’s legs are
dressed in knee-high compression stockings and sequential
compression devices to prevent the formation of deep venous
thrombosis. The patient’s feet are placed in foam booties
and the Velcro is secured loosely across the arch. Following
induction, the patient is then rotated to the contralateral side,
padded with pillows and the beanbag is put under suction to
maintain positioning of the patient. Per surgeon preference,
the beanbag is to remain under suction until the patient is
placed into the supine position. The dispersive electrode for
the electrosurgical unit is applied to the thigh, avoiding any
bony prominences, joints, implants, tattoos or scars. An axil-
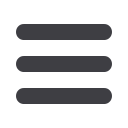
Illustrations created by Jonathan Rose, CDT
Pre op marking 002
Pre-operative marking to show where the IMF is to be recreated
after mastectomy. Midline and sternal notch identified.
Pre op marking 001
Posterior view of patient pre-operative markings. Midline and
scapula identified.

















