APRIL 2015
|
The Surgical Technologist
|
161
lary roll is placed under the down arm and the contralateral
arm placed in an airplane splint, which is abducted and rotat-
ed superiorly. This positioning allows access to the axilla for
both dissection and tunneling of the musculocutaneous flap.
Two safety straps are used to secure the lower extremities to
the bed at two to four inches above and below the knee. The
surgical gown is reversed laid across the hips and a drape is
taped to the gown and to the edges of the table. This draping
technique is used to prevent any adverse adhesive reaction
of the skin.
Following the dissection and tunneling of the latissimus
dorsi musculocutaneous flap, the beanbag will be deflated,
removed and the patient will be returned to the supine posi-
tion. The patient will need to be positioned upright to ensure
proper placement of the implant within the chest pocket and
inframammory fold. This will allow for the implant or tissue
expander to be placed with the greatest accuracy.
S K I N P R E P A R A T I O N A N D D R A P I N G
The patient’s skin is prepped beginning at the chin, extend-
ing the length of the torso to the level of the iliac crests
and down to the table at the sides including the axilla. Per
surgeon’s preference, the patient is prepped with slightly
diluted chlorhexidine cleanser. The surgical site is then blot-
ted to remove excess skin preparation solution so the drap-
ing can begin. The surgeon and the assistant drape off the
patient using blue towels, a three-quarter drape and a large
antimicrobial incise drape that has been cut into thirds. The
antimicrobial incise drape is used to affix the blue towels to
the sides and across the hips of the patient. A disposable
U-bar drape is used to drape off the lower half of the patient
and extended out to cover the lower extremities while a top
sheet is placed at the neck and secured to two IV poles by
the anesthesia provider.
P R O C E D U R E
Once the patient is properly positioned and draped, the first
incision is performed on the chest, through the previous
mastectomy scar. The scar is infiltrated with local contain-
ing epinephrine and opened in its entirety. Through this
incision the pectoralis major is released from its costal
attachments at the inframammary fold and minimally at the
inferior aspect of the sternum. Radiation has transformed
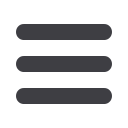
Pre op 1 reconstruction
Left latissimus reconstruction is completed. Healthy myocutaneous
flap is shown and expansion through tissue expanders is ongoing.
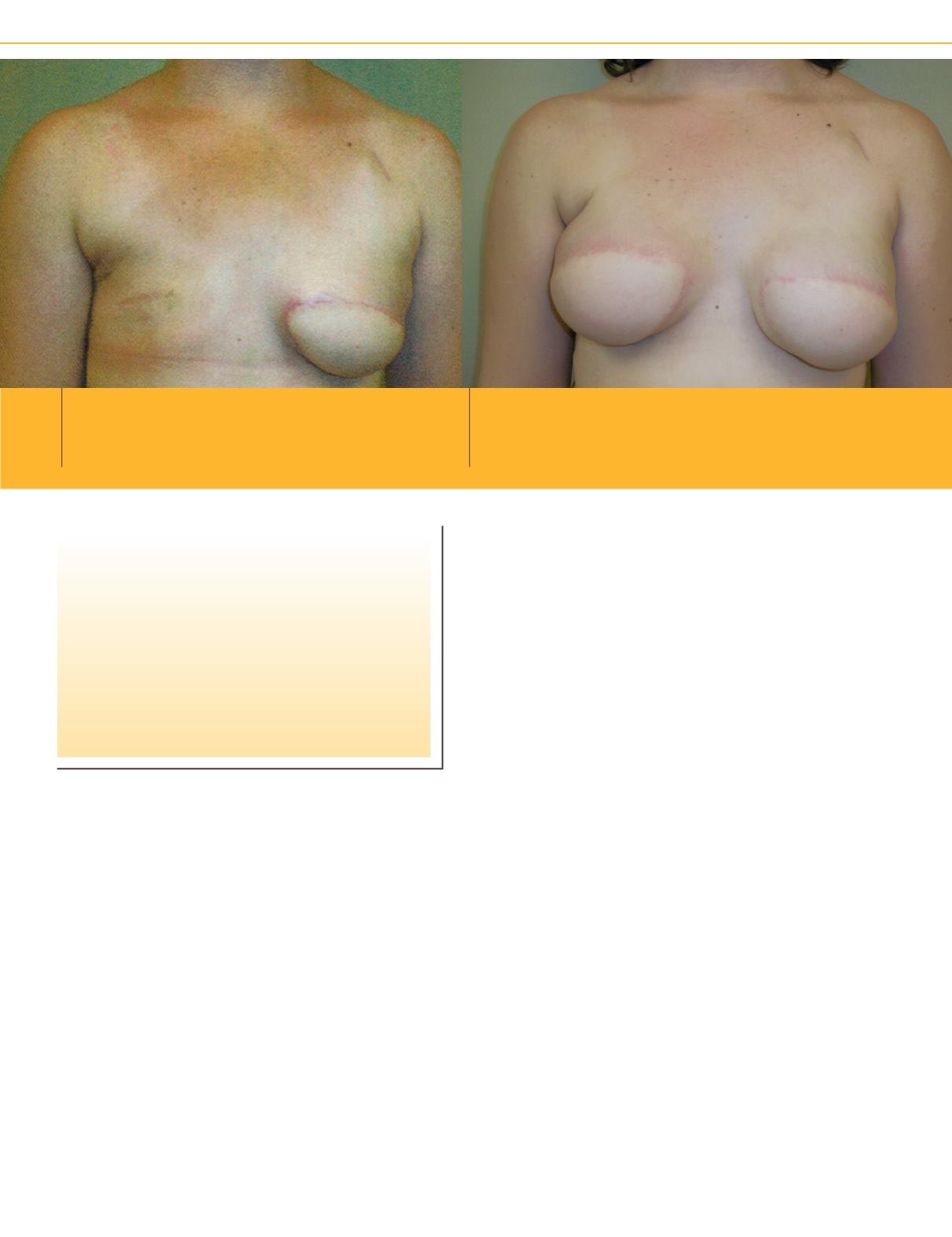
Interm
Second latissimus surgery has been performed on this patient. Both tissue expanders
have been filled to the desired size. The tissue expanders will remain in the patient for
3 months before being exchanged for implants and the nipples reconstructed.
Autologous reconstructions, such as the
latissimus dorsi musculocutaneous flap,
providepreviously irradiatedbreasts a cos-
metically acceptable outcome with low risk
when a prosthesis and a latissimus flap are
used in conjunction with each other.

















